In a startling resurgence of public health anxieties, a new virus spreads silently through U.S. dairy farms and rural communities.
It’s the H5N1 avian influenza virus—once seen as an exotic pathogen affecting poultry, now adapting in ways that experts warn could echo the early days of the COVID-19 pandemic.
The virus, having jumped from birds to mammals, is now infecting dairy cows across the United States—and even more disturbingly, people.
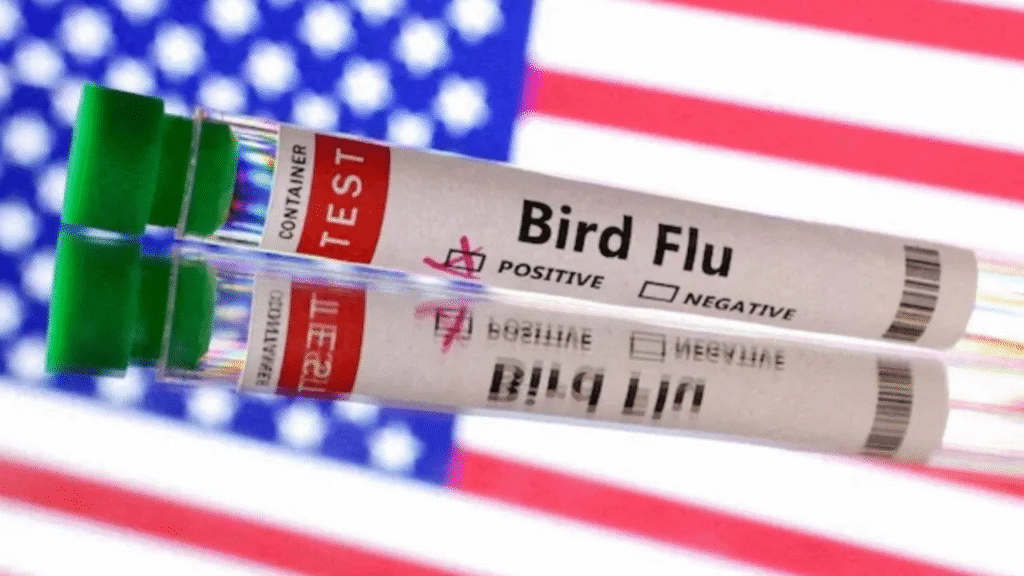
As of April 2025, the H5N1 virus has impacted more than 1,000 dairy herds across 17 U.S. states, with over 70 human infections and at least one confirmed death.
The Centers for Disease Control and Prevention (CDC) maintains that the public risk remains low. But scientists are less comforted by the numbers than by the virus’s newfound behavior—its leap across species barriers, and its potential to mutate into something far more dangerous.
The States of Concern
The outbreak, first identified in Texas dairy cattle in March 2024, has since expanded to farms in California, Kansas, Ohio, Michigan, Idaho, South Dakota, New Mexico, North Carolina, and Minnesota, among others. In an unprecedented event, the virus was also detected in raw milk samples and even feline pets on affected farms.
Until now, H5N1 was primarily seen in birds, with wild waterfowl acting as silent carriers. But the current outbreak marks the first known widespread infection of dairy cows, raising questions about food safety, agricultural stability, and zoonotic spillovers—the transmission of viruses from animals to humans.
“Each time this virus jumps species, it learns something new,” warned Dr. Marc Johnson, a virologist at the University of Missouri. “It’s not a pandemic yet, but it’s acting like it wants to be.”
Origins and Evolution
The H5N1 virus—officially classified as a highly pathogenic avian influenza (HPAI)—was first detected in domestic geese in Guangdong Province, China, in 1996. It gained international attention in 1997 when it infected humans during a poultry outbreak in Hong Kong, killing 6 out of 18 infected individuals. This marked the first time an avian influenza virus had crossed the species barrier and caused fatal disease in humans without first mutating in an intermediary mammalian host.
According to Dr. Malik Peiris, a virologist at the University of Hong Kong who was among the first to study H5N1, “The 1997 outbreak was a wake-up call. It showed us that an avian virus could directly infect humans and be lethal. That had never happened before with this kind of flu.”
Since those early cases, the virus has continued to evolve through a process known as antigenic drift—small genetic mutations that occur over time—and reassortment, where H5N1 picks up genetic material from other flu viruses. These mechanisms have enabled the virus to adapt to different hosts and become more transmissible in certain species. As a result, new strains and clades of H5N1 have emerged globally.
The Food and Agriculture Organization (FAO) and the World Organisation for Animal Health (WOAH) report that more than 300 million poultry birds have either died or been culled due to H5N1 outbreaks since 2003. In Egypt alone, one of the worst-hit countries, over 15 million poultry birds were lost during a single wave in 2006–2008, severely affecting smallholder farmers and national food supply chains.
The virus’s geographic spread has been relentless. Originally localized in Asia, H5N1 has now been reported in over 80 countries across five continents. Migratory birds have played a critical role in this transcontinental transmission. Wild waterfowl, especially ducks and geese, can carry the virus asymptomatically and excrete it in large quantities, contaminating shared water sources and infecting domestic birds.
“H5N1 has essentially found a natural reservoir in wild birds,” explains Dr. David Morens, a senior advisor to the Director of the National Institute of Allergy and Infectious Diseases (NIAID). “What makes it dangerous is its dual nature: it kills poultry at an industrial scale and still lingers quietly in migratory populations, which makes eradication extremely difficult.”
What makes the virus particularly alarming is its mortality rate in birds, which can exceed 90–100% within 48 hours of infection in some domestic species like chickens and turkeys. The financial impact is staggering: A 2022 report by the World Bank estimated that H5N1-related disruptions could cost affected economies up to $10 billion annually, including losses from export bans, vaccination efforts, and culling operations.
Furthermore, the continued evolution of H5N1 in birds—and its ability to infect mammals like foxes, cats, and even seals—raises the stakes for a potential species jump. Each new outbreak is not just a biosecurity issue but also a biological experiment in real time, increasing the risk that the virus might mutate into a form capable of sustained human-to-human transmission.
As of 2025, scientists have sequenced over 2,000 genetic variants of H5N1. Many of these variants exhibit mutations in the HA (hemagglutinin) protein that allow better binding to human-type receptors, although none have yet achieved efficient spread among people.
“We’re walking a genetic tightrope,” warns Dr. Yoshihiro Kawaoka, a renowned influenza researcher at the University of Wisconsin–Madison. “One or two mutations in the right genes—especially those governing transmissibility and receptor affinity—could change everything.”
How Did We Get Here?
The story of H5N1 began decades ago, in the live bird markets of Guangdong, China, in 1996, where the virus was first identified in domestic geese. Its deadliness was clear from the start: H5N1 could wipe out entire flocks of poultry within days. By 1997, it had infected humans for the first time in Hong Kong, killing six out of 18 people who became ill. The city responded with a dramatic culling of 1.5 million chickens—a drastic but effective measure.
Since then, H5N1 has become endemic in birds across Asia, Africa, Europe, and parts of the Middle East, causing periodic outbreaks that devastated poultry industries and killed hundreds of people. But until now, its ability to infect mammals had been limited to isolated incidents—in foxes, seals, or the occasional cat.
That changed in early 2024, when dairy cows in Texas began showing signs of illness: reduced milk production, lethargy, and fever. Initial tests ruled out common cattle diseases, but genetic sequencing confirmed the presence of highly pathogenic avian influenza. Suddenly, the virus wasn’t just a bird problem—it was a mammalian threat.
Why Are Experts Worried?
There are several red flags that have scientists deeply concerned. First, H5N1 is no longer sticking to birds. It’s now infecting mammals efficiently, a major evolutionary step. Second, human cases are increasing, particularly among farmworkers exposed to infected cattle or raw milk.
The first U.S. bird flu death occurred in January 2025 in Louisiana, when a 65-year-old man—already ill with underlying conditions—contracted the virus after contact with a backyard flock. He died from acute respiratory distress, a hallmark of severe influenza.
More recently, a child in Texas was confirmed to be infected, though their case was mild. That alone alarms pediatric epidemiologists, who emphasize that a virus capable of reaching children through indirect exposure may already be finding new pathways.
According to Dr. Sten H. Vermund, dean of the USF Health College of Public Health, “Understanding the current landscape of H5N1 infections is critical. The virus has adapted in ways that could potentially lead to sustained human-to-human transmission if we’re not vigilant.”
Genetic sequencing by the CDC has already revealed mutations in the hemagglutinin (HA) protein—which the virus uses to bind to cells—that suggest a growing affinity for human airway receptors.
And there’s another concern: viral load in milk. The USDA and CDC have confirmed the presence of the virus in raw milk samples. Although pasteurization is effective in inactivating influenza viruses, the spread of H5N1 into the human food chain raises new and troubling questions.
What’s Being Done?
Federal agencies have ramped up their response, but experts say it may be too slow.
In May 2024, the U.S. Department of Agriculture (USDA) issued a federal order requiring mandatory testing of dairy cattle before interstate transport. This measure appears to have reduced the geographic spread of the virus, narrowing the number of new affected states from 14 to just 2 within a month.
Meanwhile, the CDC has deployed flu surveillance tools to track human infections, while advising strict use of personal protective equipment (PPE) for anyone handling livestock or raw milk. Guidelines now include recommendations for vaccinating poultry workers and exploring the development of animal-targeted vaccines, though no bovine vaccine for H5N1 currently exists.
On the global stage, the World Health Organization (WHO) and Global Virus Network (GVN) have urged for international data sharing, especially around viral sequencing and cross-species transmissions. Several European countries have already restricted dairy imports from the U.S. as a precaution.
Still, gaps in reporting, limited surveillance in rural regions, and fear among farmworkers have all contributed to undercounting and misinformation.
As The New Virus Spreads, Should You Panic?
The short answer: Not yet. But stay informed and alert.
The CDC continues to reassure the public that the risk of widespread human transmission remains low—and based on current data, that is true. Most human cases have involved people with close, prolonged contact with infected animals, not casual community spread.
That said, H5N1 has shown it is a nimble, mutating virus. If it gains the ability to transmit efficiently between people—especially through the air—it could trigger a health crisis of global proportions.
This is why many scientists are now advocating for a “Pandemic Prevention Protocol”—a global infrastructure that responds to early warning signs like those seen with H5N1. The model is simple: act early, test widely, vaccinate where possible, and communicate transparently.
“We can’t afford another ‘wait and see’ approach like in 2020,” warns Dr. Angela Rasmussen, a virologist at the University of Saskatchewan. “When a new virus spreads, we need to respond like it could be the next big one—because someday, one of them will be.”
For now, experts recommend the following:
- Avoid raw or unpasteurized dairy products.
- Use gloves and masks when handling livestock or poultry.
- Report any sick animals to local agricultural authorities.
- Stay updated via official CDC and USDA channels.
The Bottom Line
As this new virus spreads—moving from birds to cattle to humans—it presents a rare glimpse into what scientists call a “species jump cascade”, where a pathogen crosses multiple biological barriers in succession. That process doesn’t happen by accident. It’s a sign that something fundamental is shifting in our relationship with the natural world.
Whether or not H5N1 becomes the next pandemic remains to be seen. But it has already reminded us of how interconnected our health systems, food supply, and ecosystems truly are. And how, in a world still recovering from COVID-19, the next threat might already be among us—one mutation away.
Read More : RFK Autism Registry: Volatile Plan in Focus
